
Since I keep mentioning Ben in my blog posts I thought I better give a little background. At the end of my pregnancy with Ben my Dr noticed I had excess amniotic fluid. We did ultra sounds and couldn’t find anything wrong but when Ben was born it was quickly obvious that something was seriously wrong. He sounded like he was trying to cry through water. I held him for just a moment before he was taken from me because he couldn’t get a good breath.

Jonathan remembers hearing the R.T. counting the seconds that Ben wasn’t breathing. Ben was trying to cry but couldn’t through all the secretions in his mouth, (we realized later he couldn’t swallow.) I still have a hard time looking at the first photos we took of his life (this one was when we were still oblivious!), he looked too blue and it just brings that sad wrenching feeling back. For the first day of his life they had to intubate him to help him breath.

Because the hospital didnt have a NICU, the doctors worked on him for about 6 hours then needed to transfer him. Watching them roll his tiny body out in the little baby incubator I was just in disbelief and shock, this was so far from what we had expected, it was so sad to see him that way. Now looking back I know there was no way we could have been prepared for how serious his condition was.

Jonathan followed the ambulance to San Juan Hospital, then slept on a bench by the NICU door because parents aren’t allowed in at night (in the ICU they have beds for us, but not the NICU.) I slept for a few hours and then headed over. I didn’t get to actually hold him for 3 days because the doctors were so unsure about his breathing. He ended up transferring again to UCDavis where they have ENT specialists. He was there for 7 weeks.

He looked so perfect, I just thought he was the most beautiful baby, and his 8lbs 12 oz size made him look like a huge pig next to all the little premies! I just loved all his rolls and check out the back fat!

His main issue was that he had an overall low muscle tone that affected his airway. He was getting stronger- starting to swallow more but we had to continuously suction his mouth because when he cried he would get overwhelmed by his own secretions, clench- and go apneac. Basically hold his breath to protect his airway. I remember watching him turn blue more than once in front of my eyes as they called a code. (It was very surreal every time.) Anytime we left the room we would listen for any “Codes” over the hospital intercom!

Because he could not eat enough to sustain himself orally (we had been feeding him through his nose,) we decided to give him a G-tube (feeding tube in his tummy) while still hoping he would continue to improve and grow out of this. We had also been walked through the idea of a trach but we were so hopeful we wouldn’t have to go that route. The night before his G-tube surgery he had two apneac episodes for no apparent reason and we realized he could not maintain a stable airway. Now I see it as a tender mercy, a signal to us that he needed more help to be safe. So he had a trach placed the same day. Here are his Before and After pics.


You can imagine how many times I kissed his little neck before that surgery. Even now its heart wrenching to look at these photos.
During his stay at UCD we did multiple tests, including every genetic test you can do (so many I cant remember them all) but all came back negative. We began to wonder if what Ben had was simply a “fluke” and he would just grow out of it. (When TY came along that theory was put to rest :).) Over the first six months he did get stronger but when he would get sick with a cold he seemed to have very little reserve. It would just take a lot out of him. One cold/flu lingered for a week and finally I took him into the ER thinking he may have a pneumonia that we hadn’t detected. He just did NOT look good. That day he coded 4 times. He was very dehydrated and had more than 100 pricks from the doctors trying to get a line. Finally after seven IO’s (needles pressed directly into the bone marrow) they did stabilize him but over the next few days all his organs (heart- liver- kidneys- bowls-) tried to shut down. He also had small brain bleeds from the trauma. I mention this all because many of the neurological delays he has now probably stem from that trauma. I also mention it because it was one of the VERY HARDEST DAYS of my life.
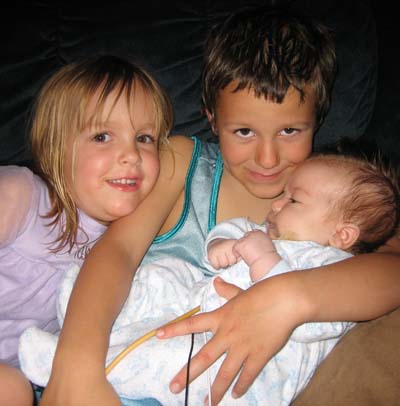
First day home! I love this photo of Jack with his arms stretched out, he was so happy to get “his baby” home, but he was still a baby himself!

We placed his equipment on a kitchen cart with wheels because he needed to be on his mist most of the time (the blue tube.)

After recovering he did continue to progress and was able to start swallowing and eating small amounts, today we still use his G-tube to supplement his diet but he can eat a large variety of bite sized foods now. Pizza, cheese and avacado are his favs.
We have tried twice to take his trach out, at 18 months and then again at 3 1/2 years old. Each time he did well for a time but then started to struggle. The first time he was trach free for 8 months, the second time almost a year before he started passing out from high levels of Co2. We now know he will have his trach indefinitely. During one of the earlier surgeries we did a muscle biopsy that showed a possibility of “mitochondrial miopathy.” which is generic for “something is wrong with your energy genes.” But now 7 1/2 years later tests are showing that may not be the case.
Here they are today, Ben is the small one. 🙂 While I have my BOO HOO moments, I am also able to be grateful for the things that are Unwritten.

Click on “Blog” on the left for more posts.